March 8, 2020 Corona Virus Update: Facts and Preparedness

When the Coronavirus was first identified in Wuhan, Hubei Province, China, I have to admit, I was not as worried about the impacts of this virus as I am today. Things have changed very quickly.
Although I am not an epidemiologist, an infectious disease expert, or a virologist, I see many patients every day where I get questions on the Coronavirus. There has been a slow response (in the US) for detection and yet a rapid increase in the patients who have now tested positive in the Bay Area, and globally, my friends and family that live in China, Italy, Japan, Iran and Korea have greatly been impacted. Now with the cruise ship with more than 3,000 preparing to dock at the Port of Oakland tomorrow (March 9, 2020), this issue is very, very real.
I have consolidated research from various physicians, scientists and health organizations in hopes of informing you so that you can be prepared. Outline below:
- WHAT WE KNOW
- WHAT WE DON’T KNOW
- PREPAREDNESS: HOME SUPPLIES
- STOP TRANSMISSION
- DISINFECT
- WHEN TO GO TO THE ER
- TREATMENTS
- VACCINATION
- OTHER LINKS
WHAT WE DO KNOW
This new Coronavirus (COVID-19) is exactly that. It is NEW. We don’t know enough about this virus yet so facts that are true today (March 8, 2020), may change tomorrow.
It is not the same as the coronaviruses that commonly circulate among humans that cause mild illness, like the common cold. A diagnosis with coronavirus 229E, NL63, OC43, or HKU1 is not the same as a COVID-19 diagnosis, with evaluation and treatments being different for these patients.
- DETECTION: The Chinese sequenced the entire DNA sequence of Coronavirus. On January 10, 2020 they shared this with the world. Like SARS, the genome sequences suggest presence of a virus closely related to the Severe Acute Respiratory Syndrome (SARS)-related CoV, where we had a 2002-2003 outbreak in humans. The virus has also been detected in many bats. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.3.2000045.
- Real-Time PCR is an easy lab technique that can be used to detect the virus and has about 95% sensitivity, meaning it will pick up the active virus if you have it, along with a high specificity, meaning cell cultures with other endemic human coronaviruses will not be picked up. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6988269/ If you test positive, you are most likely positive.
- The problem is, that PCR only detects an active and replicating virus. There are plenty of cases where negative patients turned positive and positive back to negative. This means that there is a period where positive patients have been roaming around infecting others. There was a study done in China, published on February 26, 2020, which followed 1014 patients. This showed that CT scans of the chest had better sensitivity for detecting the lesions in the lungs due to the virus before RT-PCR could detect the virusb and that patients showed improvement in chest CTs before RT-PCR results turned negative. https://pubs.rsna.org/doi/10.1148/radiol.2020200642
- Unless you test for anti-bodies, which are created once your body encounters a virus, we don’t know who was infected (ie. a carrier that spread the virus around without knowing).
- DETECTION IN THE US:
- There have been several reasons why US has been slow at detecting Coronavirus in infected people: 1) Regulatory limitations; 2) CDC Manufacturing flaw; 3) Lack of foresight. For the first 6 weeks of Coronavirus testing, the CDC only allowed testing of certain people who had recently returned from China. Now, the CDC has different guidelines, recently revised on March 4, 2020: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fclinical-criteria.html. In addition, despite the entire DNA sequence being shared with the world, and other countries such as Korea being able to test 140,000 people, the US has not had access to test kits. Why? The CDC had a manufacturing flaw related to one of the reagents (used for PCR) which caused a lack of availability for this test https://www.cdc.gov/coronavirus/2019-nCoV/summary.html#cdc-response. They are working to address this issue. In the meantime, academic and commercial labs are creating their own testing. Stanford Clinical Virology Lab has deployed a test, with the plan of being able to test 100-150 patients per day (limited to sick patients) https://med.stanford.edu/news/all-news/2020/03/stanford-medicine-COVID-19-test-now-in-use.html. UCSF has also created a test, with the capability of testing 30-100 patients per day. Unclear where it came from, but “there was clear lack of foresight,” Nathan Grubaugh, an epidemiologist at the Yale School of Public Health, says. “We were very slow to roll out testing capacity to individual places…” and we are now trying to catch-up. Despite academic and private institutions creating means for testing, the demand will continue to exceed the testing capacity in the Bay Area in the short-term.
- DETECTED CASES (as of March 7, 2020):
- United States (as of March : 164 detected cases, 11 deaths, per the 19 states that are reporting. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html
- Santa Clara County: 37 https://www.santaclaraca.gov/i-want-to/stay-informed/current-topics/coronavirus-updates
- San Francisco: 8 https://www.sfcdcp.org/infectious-diseases-a-to-z/coronavirus-2019-novel-coronavirus/#1511206332173-94eb250b-d1fa
- For reference the flu has 291,000-646,000 deaths worldwide with 12,000 to 61,000 deaths in the US per year https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-disease-2019-vs-the-flu.
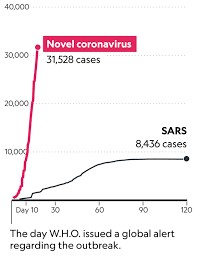
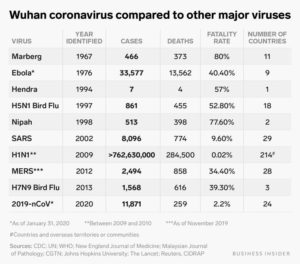
- In comparison to other viruses, we have detected many more cases within the first month of outbreak. Note we also have better ways to detect, but the number is pretty significant. https://www.sciencealert.com/this-chart-shows-how-the-wuhan-virus-compares-to-other-recent-outbreaks
- TRANSMISSION
- AIRBORNE: The virus can be transmitted trough aerosol droplets (when people cough or sneeze). The average infectious droplets size is around 5 microns, are fairly heavy and therefore not able to travel more than 6 feet. In comparison, other viruses, such as the Rhinovirus (simple cold), can travel in smaller particles for more than 10 feet.
- SURFACE SURVIVAL: The virus lives on the surface for 2-10 days. The coronaviruses, including COVID-19 have a fat-layer that protects the viral particles. The higher humidity, moderate temperature, solid surface and low wind aid in its survival.
- COVID-19 is spread primarily through contact with respiratory droplets. For example, if someone with the virus sneezes, you touch the respiratory droplets and adjust your makeup, pick your nose, and eat it while driving because (you think) nobody can see you, you can get the virus. I have read some articles that suggest it can also be airborne https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-disease-2019-vs-the-flu. Emily Landon says that most Coronaviruses are not generally airborne. https://www.uchicagomedicine.org/forefront/prevention-and-screening-articles/wuhan-coronavirus
WHAT WE DON’T KNOW
- WHEN WILL THIS SLOW DOWN?
- We do not yet know if warm weather will stop the outbreak like SARS https://www.cdc.gov/coronavirus/2019-ncov/faq.html
- WILL THIS TURN INTO A PANDEMIC?
- The WHO has been very cautious to use the word pandemic. Nonetheless, this virus is spreading rapidly world-wide, and there have been many comparisons to the Spanish Flu Pandemic in 1918, that lasted a few months and affected 50-100 million people world-wide and 675,000 people in the US. There’s a big difference from that 1918 outbreak, in that within 2 weeks, scientists identified the Coronavirus and sequenced its genome and discovered the likely origin. In 1918, they also had no antibiotics, which can kill bacterial infections that can follow viral infections. We also have hospitals with ICU, faster detection methods, and ways of supporting very sick patients. These are positive things!
- The problem is, that our health care system does not have “surge” capacity”, meaning during this flu season where ICU’s are already often at full capacity, we will not be able to keep up with the addition of severely ill people from the new Coronavirus. https://www.wbur.org/commonhealth/2020/03/02/infectious-disease-doctor-coronavirus
- Whether “pandemic” is the term that the WHO decides to use for current Coronavirus status, we have a problem that is going to grow exponentially before it gets better.
- FATALITY:
- The top Chinese health official, Liang Wannian stated that in China, the fatality rate was 3-4%. However, if you factor out all the data from Hubei province (where Wuhan is located), the fatality rate in China drops to 0.4%. Wuhan was one of the first places that got affected, and health care providers did not know what they were dealing with. With subsequent infections, and after the genome was sequenced, the other Chinese provinces knew how to diagnose, treat and support this illness https://www.npr.org/sections/goatsandsoda/2020/03/03/809904660/why-the-death-rate-from-coronavirus-is-plunging-in-china.
- The mortality rate estimate per the WHO as of March 3, 2020 is 3.4%. It is important to note that there are lots of kids and healthy people running around with no symptoms or light symptoms. Taking this into account, the rate is likely lower (in my opinion).
- HOW SICK WILL I GET?
- 80% will have mild symptoms: Based on a publication by China on the Chinese CDC, where 72,314 individuals diagnosed with COVID-19 as of February 11, 2020 were included in this analysis. The data shows that children < 10 years of age do not die and 81% of those exposed get mild cases. 1.2% of the cases were asymptomatic http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51. There is a chance that there is a greater percent of people that will only get mild symptoms, as we have not been able to detect everyone who has the virus and there are asymptomatic patients roaming around.
- Symptoms: Similar to the flu, the Coronavirus can cause fever, cough, body aches, fatigue, and sometimes vomiting and diarrhea. Both can result in pneumonia https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-disease-2019-vs-the-flu.
PREPAREDNESS: HOME SUPPLIES
Santa Clara County has recommendations on having supplies, prescription medications, non-prescription medications.
- Santa Clara County Public Health https://www.sccgov.org/sites/phd/DiseaseInformation/novel-coronavirus/Pages/home.aspx
- Public Call Center: 408-885-3980
Below are suggestions of what to have what to have at home:
- Minimum 2-4 week supply of water and Food. We have an earthquake food supply bucket, but in addition, stocked up on Annie’s Organic Soups, nuts, sauces, gluten-free and glutenous pastas, Emergen-C, teas, dried fruit, tuna, organic chicken bone broth. Think: easy food you will want to eat if you are sick or in lockdown.
- 1 month supply of prescription drugs
- Tylenol, ibuprofen, electrolyte packets, vitamins
- Household supplies: soap, antibacterial wipes, hand sanitizers, bleach, rubber gloves, disposable face masks, tissues, toilet paper, ladies sanitary napkins.
- Disinfectants: To disinfect, ethanol > 70% should be used or a 1:50 dilution of bleach should be used. Look at the bleach % on the bottle. Think: how to sanitize your house if your loved one tests positive.
- Plan: Come up with a plan for if someone does become sick in your household. If you have elderly parents without caretakers, stock them up with supplies in advance.
STOP TRANSMISSION
- If you are >50 (with highest risk category people > 80), immune compromised, have respiratory issues, avoid crowded areas. This virus can travel 6 feet, so you can be friendly from a distance.
- Work from home if possible and minimize travel.
- Masks: I have read “don’t wear a mask unless you know you are sick.” This makes no sense to me since many people have minimal symptoms and don’t know they are infected. I would like to counter-propose, if you think you are sick, wear a mask! Yes, the virus can still be transmitted through mucosal membranes (such as your eyes) but we know that your virus-containing respiratory droplets are contagious so why not cover your nose and mouth which is more than half the entryways from your face? Masks are sold out or too expensive? Wear a scarf.
- Cough into your elbow, not your hand.
- Start practicing not touching your face (I just touched mine after I typed this). It’s not easy.
- Wash your hands for 20 seconds, as if you have the Coronavirus on your hands, in your fingernails and on your arms.
DISINFECT
- The SARS virus, which is similar to COVID-19, at a temperature of 68F (20C), lasts 2 days on steel, 4 days on wood/glass, 5 days on metal/plastic/ceramics. These researchers also found that one strain of SARS lasted up to 9 days on plastics. SARS survives 2-8 hours on aluminum, less than 8 hours on latex. It can survive for 5 days on Teflon (your pots and pans). A concentration of 70% ethanol, or a standard bleach dilution of 1:50, or a dilution of 1:100 of 5% sodium hypochlorite (final concentration 0.05%) is effective in disinfecting small surfaces https://www.journalofhospitalinfection.com/article/S0195-6701(20)30046-3/fulltext. We can extrapolate that if it’s good enough for SARS, it’s good enough for COVID-19 (till further notice).
- Many alcohol-based hand sanitizers do not have an alcohol content high enough to disinfect from COVID-19. Check if it’s at least 70% alcohol.
- Disinfect: phones, keyboards, door knobs, sinks, toilet handles, things that you touch every day at work and at home. Doctor’s don’t forget about your stethoscopes!
WHEN TO GO TO THE EMERGENCY ROOM
- “Only people with symptoms of severe respiratory illness should seek medical care in the ER. Severe symptoms are rapid heart rate, low blood pressure, high or very low temperatures, confusion, trouble breathing, severe dehydration. Call ahead to tell the ER that you are coming so they can be prepared for your arrival.” Dr. Todd Ellerin, Harvard Medical School https://www.health.harvard.edu/blog/as-coronavirus-spreads-many-questions-and-some-answers-2020022719004
- The incubation period, the time between catching the disease and beginning to have symptoms disease is estimated from 1-14 days, on average 5 days, per the WHO. The at-risk population are the elderly, people with other medical conditions (ex. Lung disease, heart disease, cancer, diabetes). https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
- For clinicians, here are the guidelines from the CDC for reporting persons under investigation https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fclinical-criteria.html
TREATMENTS: ANTI-VIRALS
- Antiviral medications are currently being tested to see if they can address symptoms. There are various pharmaceutical companies looking into this.
- The WHO says that Gilead’s Remdesivir (the drug developed for Ebola), may have efficacy in treating COVID-19. There are two trials at the moment with results anticipated in April 2020. Other sources claim there is a 50/50 chance of success https://www.bloomberg.com/news/articles/2020-03-05/gilead-analyst-sees-only-50-chance-that-coronavirus-drug-works
- The University of Chicago found drugs previously in development for SARS that could be effective for COVID-19 https://www.uchicagomedicine.org/forefront/prevention-and-screening-articles/wuhan-coronavirus
- Tamiflu (used to shorten the flu symptoms) is not a treatment for COVID-19. Also, antibiotics will not work to treat COVID-19!
VACCINATIONS
- Per Infectious Disease specialist, Dr. Amy Landon, the vaccinations can be expected around spring 2021 at the earliest https://www.uchicagomedicine.org/forefront/prevention-and-screening-articles/wuhan-coronavirus.
- This is a good opportunity for me to put in a plug for other vaccinations, for those parents still on the fence about vaccinating their children from preventable diseases!
OTHER LINKS
- UCSF guidelines for the San Francisco Community https://www.ucsf.edu/coronavirus
- Kaiser Facts vs Fears: https://khn.org/news/facts-vs-fears-five-things-to-help-weigh-your-coronavirus-risk/
- HARVARD FAQ’s: https://www.health.harvard.edu/blog/as-coronavirus-spreads-many-questions-and-some-answers-2020022719004
- CDC’s PRE-PANDEMIC CHECKLIST: https://www.cdc.gov/nonpharmaceutical-interventions/tools-resources/planning-guidance-checklists.html
- CDC Global Planning to reduce the impact of a pandemic https://www.cdc.gov/flu/pandemic-resources/planning-preparedness/global-planning.html
Know your facts, have a prevention plan, have a plan in case someone in your household gets infected. It pays to be proactive and not reactive in a frenzy.
Here is to everyone staying healthy,
Dr. Mikiko Murakami